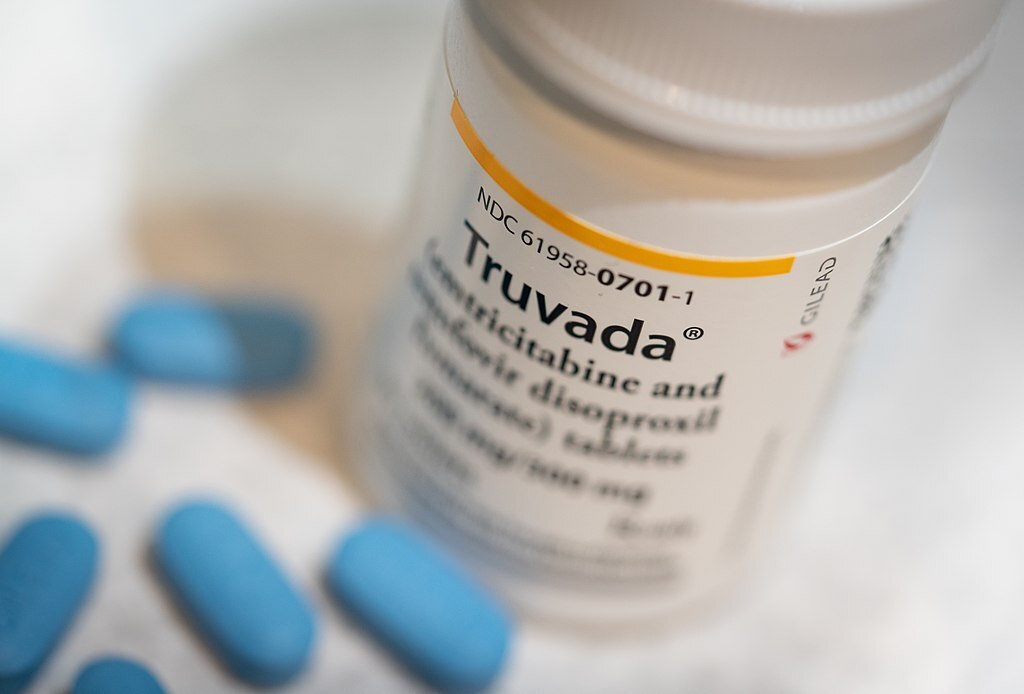
Image credit: Tony Webster
A huge change happened for customers of health insurer UnitedHealthcare yesterday, Sept. 1, as the insurer requires its policy holders to switch to Truvada as they are no longer covering payments for the pre-exposure prophylaxis (PrEP) drug Descovy.
MedCity News reports that people on Descovy would have to talk to their doctors to either switch them to using branded Truvada or its generic version that is meant to arrive on the market by Sept. 30. People taking Descovy who intend to continue doing so will have to pay higher and acquire a prior authorization.
UnitedHealthcare policy holders who decide to go with the generic version of Truvada instead will be able to acquire it with no out-of-pocket cost.
The move by the insurer could have widespread effects on people on PrEP. While Truvada and Descovy are both made by pharmaceutical company Gilead Sciences and have the same effectiveness, Descovy has fewer side effects than Truvada. Compared to Truvada, users of Descovy suffer less incidents of kidney function loss and do not lose as much of their bone mineral density.
Gilead said that a decision like the one UnitedHealthcare made could “further complicate an individual’s decision to use PrEP and jeopardize ongoing efforts to curb new HIV infections and end the epidemic.”
However, MedCity News quotes University of Michigan’s Center for Value-Based Insurance Design director Dr. Mark Frederick as saying that the decision might actually convince more people to go on PrEP as there will be no cost-sharing should they decide to use the generic version of Truvada.
According to Frederick, offering more people a lower-cost drug at zero cost sharing is a trade-off that he would be willing to make, especially if he were a government body like the New York City health department.









This revelation is neither good nor bad.
It is a trade-off between availing a drug/drugs and sustaining profits. It is envitiable that the drug manufacturers are going to remain viligant about profits without encouraging a backlash.
It is simply… six-of-one; a half-dozen-of-the-other. It is a reflection of captialism with its supply-demand economy. The Public will adjust as it always does as some things are elastic while other things are unelastic.
Brand-name drugs are elastic…particularly…after their patents expire and a gneric substitue is manufactured. Hence, the generic equivilent will be just a suitable if with a somewhat more delirious side-effects?
Every economic and healthcare system has a finite amount of resources. Even if we had single payer healthcare or were a socialist economy, it is likely that the use of Descovy would be limited when the majority of people will do just fine with Truvada or its generic.
It would be handy to know the kidney complication rate of both drugs before commenting but, on the face of it, I’m not fond of the move though I’m not on PrEP.
The Intelligence in your is so attractive.
Clearly Gilead are whining because the generic Truvada brings MUCH less profit than the ‘new drug’ Descovy. Truvada is not that dangerous.
ummm A> not that dangerous is a bunch of BS. For those of us who were on Truvada and saw our kidney values suffer, I’d have to disagree; B> If generic Truvada works fine, but if there is a medical condition that requires use to use Descovy so we can continue being protected, insurance should cover it. If I was on Truvada and wanted to stay on brand name vs. generic – then it’s on me to pay the $$. But I don’t have that choice.
$60 per pill. The price of Truvada has tripled over the last few years, representing no additional value. The entire healthcare system, every person who pays his premium or can get the government to pay for you is paying for this cost. Considering nobody is supposed to be out there having sex these days, the price increase and the availability of a generic drug means a lot more people will be treated for the same cost.
Maybe the money saved can be put towards vaccine research, it’s been a long time since Dr. Fauci promised that would be coming….
Dr. Fauci never “promised” that a vaccine would be found. They might be “optimistic”, but no credible medical professional would make such a promise.
Perhaps you should qualify that as “random sex.” There is nothing wrong with people in relationships, especially if they already live in the same household, continuing to have sex. In addition, many of them may be in serodiscordant relationships where it is important for both to continue their medical regimens.
If you have health insurance the cost is much less. The price went up to $1 a pill in january for BC/BS Federal Plan subcribers. Gilead also has a copay coupon(?) program to defer the copay expense for those who qualify. I dont qualify but $360 a year is a small price out of pocket for me to avoid an HIV infection. The generic will make the drug available to many more people. I’ve never had a side affect to any prescription so I guess I am lucky.
The assertion that Descovy has fewer side effects than Truvada is false. The truth of the matter is that Descovy has DIFFERENT side effects versus Truvada.
Furthermore, I think both drugs have something big in common: users typically have a cornucopia of other STDs present in their systems thanks to the carelessness wrought by PReP.
“Typically”? That’s a broad assertion. I’ve been on PrEP for several years, and I haven’t had even one STD in my life, let alone a “cornucopia” of them.
Like I’ve been saying, just use a fucking condom or some other form of anal stimulation,. i.e. prostate massage, if you can get-over this, bottom-top thing, do each other. Gonna have to learn new tricks either way you slice it, ’cause the pharmaceuticals giants have plans for you. . . where your over a barrel.
OMG! I just up-voted you without looking at the name. Imagine my shock once I noticed who I was up-voting. Oh well, when you’re right, you ain’t wrong.
Lmao, uh, oh, what have you done-what are people going to think? In this case, it’s an olive branch, for good ole’ (what I call conservative) and common sense for survival.
As always thanks for the informative article Dave.
It’s a doctor-patient choice, not the pharmacy or an insurer. UH does not control this relationship, and I hope the lawyers get rich over the subsequent litigation.
There will be no litigation. The concept of formularies, preferred drugs and differing copays is well-established. The article mentioned that Descovy will require prior authorization (also well-established for expensive medications), which means that UHC has implemented medical criteria for its use so it will still be covered for those who meet the standards. UHC also isn’t interfering with the doctor-patient relationship because there is nothing stopping the physician from prescribing Descovy and the patient filling it outside the health plan.
It’s insane they’re peddling this toxic shit like some kind of panacea. https://www.drugs.com/sfx/truvada-side-effects.html
PrEP is nothing but another way of saying “I engage in anal sex with strangers without using condoms” Further, it seems that gay/bi men on PrEP have more sexual partners than those who are not on the drug. In short, PrEP has given gay men a license to be irresponsible. You still can contract hepatitis and other STDs from anal sex, especially hepatitis C. I have not been having sex since the pandemic. However, before the pandemic, I stayed away from men on PrEP
PrEP is also another way of saying “I understand that condoms fail, so this is another way of taking care of myself.”
I don’t know if that’s true, but the cause-and-effect is impossible to determine. Men may be taking PrEP because they have more sexual partners. And, so what if they do? Why are gay guys so judgemental? I think that some would be happier as evangelicals so that they could judge everyone.
Using a condom, is another way of saying, ” might have forgotten to take the pill.” Condom usage takes care of anything you might otherwise catch with anal-sex.
Truvada shoved my kidney numbers into the danger zone. Descovy brought them back down. This is fucked up.
Although the article buries that fact, there is a prior authorization process for obtaining Descovy for those who have a medical reason for it.
Using PreP is a lifestyle choice. Insurance companies should only be required to pay for illness. If someone wants to use Descovy for PreP, then they should pay for it. If the insurance company is offering to cover Truvada for no out-of-pocket cost, then consider it a gift. Society is not obligated to pay for sexual activity…. this is similar to the use of viagra/cialis for sexual recreation.
PrEP is cheaper than a lifetime of HIV treatment.
Hmmm…. lifetime cost of PrEP versus lifetime cost of HIV treatment using similar meds. Cost is about the same.